Micronodular Basal Cell Carcinoma - Mohs Case by Dr. David B. Roy, FAOCD, FAAD
Dr. David Roy • July 8, 2019

Primary basal cell carcinomas are classified as superficial, nodular, micronodular, and morpheic/infiltrative. Anatomical and histological characteristics of the basal cell carcinomas subtypes vary with each classification. This month’s Mohs Case presentation is a micronodular basal cell carcinoma. Micronodular basal cell carcinoma may be more difficult to eradicate and prone to recurrence than nodular subtype. Micronodular basal cell carcinoma is thought to have a greater potential for clinically surreptitious tumor spread compared with the majority of basal cell carcinomas that are nodular. They also have wider and deeper tumor extensions than nodular basal cell carcinomas of similar clinical size. The number of surgical stages required for complete removal of tumor, the width of tissue required to remove subclinical extension of tumor, and the depth of defect at completion all tend to be greater with micronodular basal cell carcinomas when compared with nodular basal cell carcinomas regardless of whether cases were primary or recurrent. All of that to say, micronodular BCCs can be significantly more destructive than nodular BCCs because tumor extension is difficult to detect clinically. When treating micronodular BCC, clinicians should keep in mind its potential for clandestine invasion.
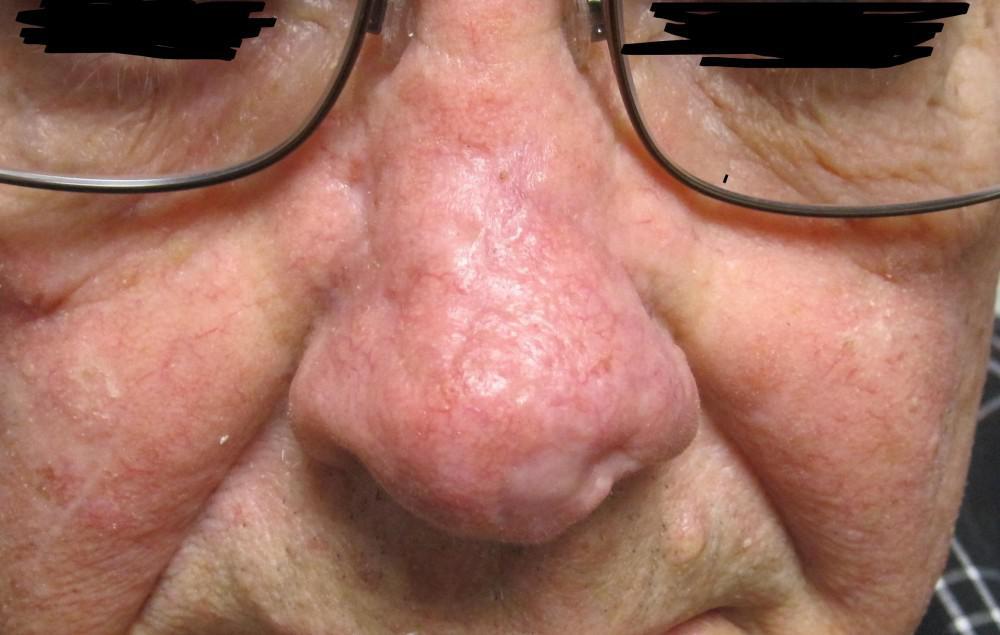
A 72 year-old male patient presented with a biopsy proven micronodular basal cell carcinoma on the right side of his nose (Figure 1). He stated that the lesion had been present for approximately one year and would heal at times, only to become raw and bleed. After discussing treatment options including Mohs surgery, radiation therapy, and oral targeted therapy, the patient decided that Mohs surgery would be the best option due to its high cure rate. Two stages of Mohs micrographic surgery were required to clear the tumor. (Figure 1). This left a significant defect to be repaired.
After discussing several closure options, including a flap and graft closure, the patient and I decided upon a transposition flap from the left side of his nose. This procedure involves lifting a piece of tissue from one area and moving it over normal tissue to fill the defect. In this case, a triangular piece of tissue from the left side of the nose was lifted and transferred over the normal skin on the middle part of the nose to fill the hole on the left side. This allowed for a single stage procedure, excellent tissue match in terms of skin texture and color, and relative quick healing time (Figures 2 and 3).
After four weeks, the patient was seen for a wound check with excellent early results (Figure 4).

Your skin, the body's largest organ, is a vital indicator of your overall health. Changes in its appearance can signal underlying medical conditions that may require attention. Whether it’s ensuring you’re getting the right nutrients, managing stress, or seeking professional care, being attuned to what your skin tells you makes it easier to stay on top of your health.

Achieving healthy, glowing skin begins with an effective cleansing routine. However, small mistakes can disrupt your skin’s natural balance, leading to irritation, breakouts, or premature aging. Avoiding these common errors and incorporating advanced techniques can significantly impact your skincare journey.

You’ve likely felt it in your life: that uncomfortable feeling of tightness, flakiness, and sometimes even itchiness that can make your skin look and feel less than its best. But what exactly causes dry skin, and how do you treat it? Don’t fret because we’ve put together some treatment tips that can help your dry skin regain its moisture.