The Many Forms of Atopic Dermatitis & A Treatment Plan For It
Dr. David Roy • April 5, 2017
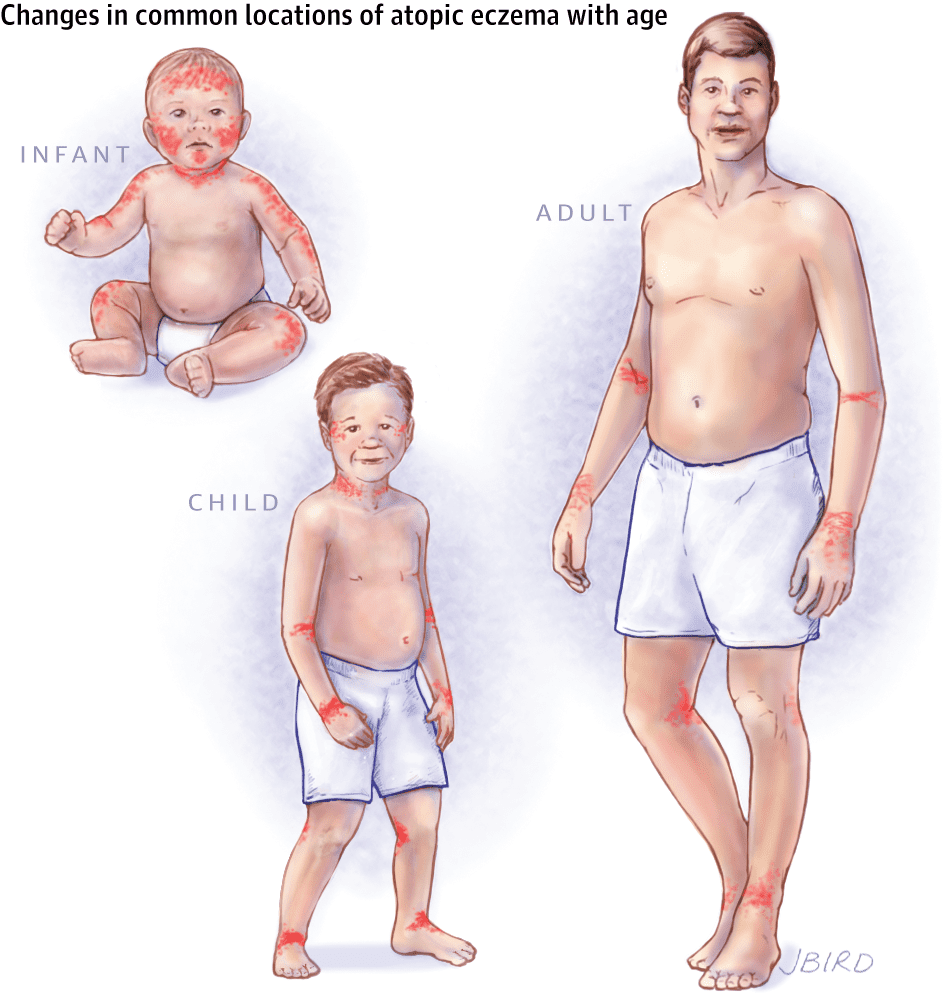
Atopic dermatitis (AD) is more commonly known by another name – Eczema. While AD is a form of eczema, eczema has come to describe other conditions that are distinct from AD. Thus we will use the term atopic dermatitis within this article in order to specify a distinct form of eczema. AD is an extremely itchy skin disease that typically starts in early infancy. While children are commonly affected, adult and adolescent atopic dermatitis is not unheard of. Atopic Dermatitis can be associated with other skin diseases such as an acute allergic reaction to a foreign object, hives, asthma, and allergic rhinitis. It is characterized by red, scaly lesions, dry skin, pruritus, and thickening of the skin (lichenification). The prevalence of AD has increased over the years and is associated with an enormous burden on patients and families. Interestingly, the development of AD can precede the development of other allergic diseases such as asthma, food allergies, and allergic rhinitis. This has led physicians and researchers to believe that early atopic dermatitis and/or cutaneous sensitization to environmental allergens may lead to other forms of allergic diseases that irritate other epithelial tissues. Examples of other tissue systems that could later become irritated by allergens include respiratory tissue and gastrointestinal tissue. Numerous studies have been done that support the suggestion that there is an association between atopic dermatitis and allergic reactions in these other tissue groups. As mentioned previously, the condition is most common in infants, but it is not uncommon for the skin condition to be present in older children as well as adults. PBD providers wanted to further discuss the different ways that atopic dermatitis may present itself in patients of different ages (i.e. different signs & symptoms):
Infants: atopic dermatitis is most common in infants with some cases appearing as early as 2-3 months of age. This early onset of atopic dermatitis often causes:
A rash of rapid appearance. The most common locations that this rash will form is on the cheeks, face, and scalp although it can appear on other areas of the body as well. This rash is irritating to the skin because it causes it to become dry, scaly, and itchy. The rash can sometimes bubble or ooze fluid.
Often times the infant may scratch the itching by rubbing on the carpet or in their crib. In addition, the children may pinch the skin of their chest, using pain to distract themselves from the itch.
The baby may have trouble sleeping because of the rash.
If the rash is scratched, it can cause the skin in the area to become infected. While parents can’t completely prevent the baby from scratching the irritated surface, they should schedule an appointment with PBD to alieve the child of the frustrating itch.
Children: If a child develops atopic dermatitis between 2 years of age and the years they are going through puberty, they often will exhibit the following signs and symptoms:
The atopic dermatitis in patients that fall within this age group may experience a rash that starts in the creases of their knees or elbows. It is not uncommon for the rash to appear on the wrists, ankles, feet, or the crease between the buttocks and legs.
In the area where the rash appeared the skin may become scaly and itchy.
The skin with atopic dermatitis in this demographic can vary in appearance:
Can appear as small bumpy patches. Some patients describe them as looking like “permanent goose bumps”.
The area where the rash appeared can become discolored (lighten or darken).
It may become rough, thick, and/or leathery. Often times this can be the result of countless attempts to scratch the itchy spot.
If the rash occurred in an area with thick skin, knots may develop beneath the skin.
The thick skin effected by the rash may itch all of the time rather than every-so-often. The thick skin can itch even when there is no atopic dermatitis flare up.
Adults: It is rare that adults have atopic dermatitis, in fact, only around 10% of atopic dermatitis patients are over the age of 5. Nonetheless, it is a condition that can appear in adults and the symptoms associated with adult flare ups differ from those in infants and children. Signs and symptoms of adults include:
- Rashes appear on the neck and in the creases of knees and elbows.
- Rashes are large and can cover much of the body.
- Rashes can be intense around the eyes in adults.
- Skin in the area where the rashes appear can become extremely dry and can become much more scaly than in infant and child patients.
- Patients may experience a non-stop itch.
- May lead to skin infections in the atopic dermatitis areas.
- In patients who have had a case of atopic dermatitis for a long duration of their lives, the areas where they experience flare ups can become leathery and thick due to years of scratching.
Once the diagnosis of AD has been established, patient/parent education and a strict treatment regimen must be instituted. One of the key components of any good AD care plan is treatment utilizing a technique known as wet wraps. Wet wraps have been a mainstay of therapy for decades and are an extremely effective way to improve even severe atopic dermatitis in patients of any age. The biggest hurdle that must be overcome is the amount of work and dedication that needs to be committed to make this therapy successful.
So how do wet wraps work? Immediately following application of topical prescription therapy such as topical steroids, wet dressings are applied to the skin. These can take the form of wet towels, or wet clothes. Long sleeve pajamas work fantastic. The child is allowed to play for 45-60 minutes and then the wet dressings are removed and emollients are applied. It is required that this process be repeated at least twice daily.
If performed correctly, even patients suffering from severe atopic dermatitis should demonstrate significant improvement in 3-10 days. Patients who do not show signs of improvement and who have performed the technique appropriately and consistently must be evaluated for alternate diagnoses. These include but are not limited to immune deficiency syndromes, cutaneous lymphoproliferative disorders such as mycosis fungoides, autoimmune disease, and eczema herpeticum.
A detailed care plan can be found at the end of this post. With appropriate therapy and strict patient compliance, pediatric AD patients can be managed effectively with relative ease. Those patients who do not respond will need further work-up and referral to a specialist. For further tips, visit the link below to the American Academy of Dermatology website:
https://www.aad.org/dermatology-a-to-z/diseases-and-treatments/a---d/atopic-dermatitis
Atopic Dermatitis Care Plan (Eczema)
Bathe or Shower daily in lukewarm water, for no more than 5-10 minutes, with a mild skin cleanser such as unscented Dove, Cetaphil, CeraVe, Purpose, Eucerin Gentle Hydrating Cleanser, Aveeno non-soap cleanser, or Oil-of-Olay Complete Unscented soap-free cleanser. Immediately after getting out of water PAT, do not RUB, dry with a soft towel.
Shampoo scalp __________ TIMES PER WEEK with a mild baby shampoo. For extreme flaking, use T-Sal or Head and Shoulders (dark blue bottle) or Selsun Blue or Nizoral shampoo. Leave on 5-10 minutes then rinse well.
Apply a thin film of topical prescription medication TWICE A DAY to the AFFECTED AREAS: (RED, ROUGH, RAISED, DRY AREAS ONLY) for 2 weeks then stop for 2 weeks.
Hydrocortisone 2.5% Lotion / Ointment Triamcinolone Cream / Ointment
Cutivate Lotion / Ointment Derma-Smoothe Oil
Elocon Cream / Ointment Topicort Cream / Ointment
Locoid Lipocream / Lotion Desonide Cream / Ointment
Betamethason Valerate Cream / Ointment Other Steroid: _______________
Protopic Elidel
Apply moisturizer to the entire body immediately after the topical Rx medications, and frequently throughout the day. For infants, applying moisturizers all over with every diaper change is appropriate. Vaseline is the best and the cheapest. Never apply moisturizers immediately before or after a medication application as this can decrease the effectiveness of the medication.
Ointments: Petroleum Jelly, Vaseline, Aquaphor Healing Ointment, A&D Ointment
Thick CREAMS: Cetaphil (in 1lb jar), CeraVe, Eucerin Eczema, Cetaphil Restoraderm, Aveeno Eczema Care, and Creamy Vaseline.
Antihistamines are used to decrease the itching, which helps in the overall eczema process. The dose can be adjusted up or down depending on the response. Not all patients need to use antihistamines.
Recommended: NONE Other: ____________________
Topical antibiotics may be needed if there are many cracks in the skin. This helps treat, or prevent, a secondary infection as well as help in the healing process.
Recommended: NONE Other: ____________________

Your skin, the body's largest organ, is a vital indicator of your overall health. Changes in its appearance can signal underlying medical conditions that may require attention. Whether it’s ensuring you’re getting the right nutrients, managing stress, or seeking professional care, being attuned to what your skin tells you makes it easier to stay on top of your health.

Achieving healthy, glowing skin begins with an effective cleansing routine. However, small mistakes can disrupt your skin’s natural balance, leading to irritation, breakouts, or premature aging. Avoiding these common errors and incorporating advanced techniques can significantly impact your skincare journey.

You’ve likely felt it in your life: that uncomfortable feeling of tightness, flakiness, and sometimes even itchiness that can make your skin look and feel less than its best. But what exactly causes dry skin, and how do you treat it? Don’t fret because we’ve put together some treatment tips that can help your dry skin regain its moisture.