Mustardé flap for Primary Nasal Sidewall Defect Post-Mohs Micrographic Surgery
Mustardé flap for primary nasal sidewall defect post-Mohs micrographic surgery
Sunny B. Patel, OMS-IV, Benjamin R. Buttars, OMS-IV, David B. Roy, DO
Hattiesburg, Mississippi and Dothan, Alabama
Introduction
Keratinocyte carcinoma occurs commonly on the face, owing to repeated exposure to ultraviolet radiation.1 Mohs micrographic surgery is the gold standard for treating these cutaneous tumors.2 This procedure provides margin clearance while preserving the surrounding tissue. However, large defects, especially those involving nasal tissue, can pose challenges for repair.
During repair, maintaining anatomic integrity for function and cosmesis is critical. Several techniques, including partial primary closure with secondary intention, full-thickness grafting, and flaps to achieve surgical repair, have been used to close sidewall defects. In nasal defects that are greater than 2 cm in size, surgeons typically avoid primary partial closure with an area left to heal by secondary intention due to increased challenges in healing.3 These defects often require grafts or flaps for repair. Although grafting can be used, it is associated with the risk of indentation as well as changes in tissue texture and pigmentation depending on the harvesting site.3,4 Flap repairs have the structural benefits of grafts while preserving the vascular supply, texture, and color of the original tissue. Additionally, flaps have the added benefit of redistributing tension lines around defects.5 A postoperative retrospective study showed that flap repair resulted in greater patient satisfaction, better tissue coordination, improved skin color, and shorter lengths of hospital stays when compared to grafting.3
Among the standard flaps used to treat large nasal defects, the paramedian forehead flap may be considered the “primary workhorse,” though other options exist.4 The Mustardé flap, a large, rotational flap, was initially designed to repair the lower eyelids, the cheeks, and even the nasal ala. By dispersing tension planes, it decreases the risk of ectropion, or eye sagging.5 It begins with an incision superior to the lateral edge of the primary defect, extending along the lower eyelid to the lateral canthus, followed by an incision superior-lateral to the temple region. A combination of undermining and suturing is performed to advance the tissue and close the defect.5 The literature shows no instance in which this large transposition has been utilized to cover a defect upon the nasal sidewall. This case series illustrates 3 patients who underwent Mohs micrographic surgery for cutaneous skin lesions and were left with substantial defects on the nasal sidewall or dorsum. Mustardé flaps were advanced to repair the primary defects and preserve the functionality and aesthetics of their noses.
Case series
Three patient cases were reviewed retrospectively. All 3 patients gave informed consent to be included in this case series. Each case involved a primary defect extending to the nasal sidewall, nasal dorsum, or both.
Case 1
A 72-year-old woman presented with a basosquamous carcinoma located on the left nasal sidewall, measuring 1 cm × 1.5 cm. Three stages of Mohs micrographic surgery were required to clear the tumor. The final defect size measured 1.7 cm × 2.5 cm and involved the muscular fascia. A secondary, nodular basal cell carcinoma measuring 0.8 cm × 1.2 cm was noted and treated at the time of surgery. This lesion was cleared following 2 stages of surgery to the level of the deep subcutaneous tissue and had a final defect size of 1.2 cm × 1.7 cm. The final defects involved the left nasal sidewall, medial cheek, and left infraorbital cheek (Fig 1, A).

Case 2
A 78-year-old woman presented with an infiltrative basal cell carcinoma located on the left nasal sidewall/medial cheek. The preoperative lesion measured 1.2 cm × 1.9 cm. Clearance was obtained after 4 stages, leaving a defect to the level of the periosteum, measuring 2.8 cm × 3.1 cm, with the involvement of a small portion of the nasal dorsum, left nasal sidewall, medial cheek, and medial canthus (Fig 2, A).

Case 3
A 71-year-old woman presented to the clinic with a recurrent, infiltrative basal cell carcinoma located on left nasal sidewall/alar crease measuring 1.5 cm × 1.4 cm. Clearance was obtained after 4 stages, leaving a 3.2-cm × 2.9-cm defect on the left nasal dorsum, sidewall, and alar groove, with involvement down to the fascia, deep subcutaneous layer, and perichondrium (Fig 3, A).

Multiple options for repair, including grafting, partial closure with healing by secondary intention, a paramedian forehead flap, and the use of a Mustardé flap, were discussed with the patients. All patients elected to be repaired by Mustardé flap to avoid any delayed or multiple-stage closures. For each patient, as is common with this flap, the medial aspect of the flap was elevated in the plane of the midsubcutis to match the relative depth of the corresponding defect. However, to ensure perfusion, the lateral aspect of the flap was dissected to the deep subcutis. The superior horizontal incision along the lid margin was extended laterally toward the preauricular area until sufficient tissue was mobilized to cover the defect.
Specific Modifications
A few specific, yet essential, modifications to the original flaps were required. By placing a 4-0 polyglactin suture on the zygomatic arch fascia while the medial portion of the flap was advanced to cover the defect, no tension was placed on the lower lid, decreasing the risk of ectropion. The location of the anchoring suture along the arch was selected based on the ability of the medial flap to lie “loosely” upon the lower eyelid and defect. For the remaining subcutaneous sutures (also 4-0 polyglactin), it was important that the tension vector was directed from the preauricular area to the mandibular cheek area, preventing excess tension on the medial aspect of the defect and the eyelid (Fig 4, B).
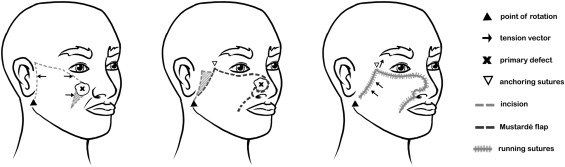
For all patients, 5-0 nylon epidermal sutures were placed (Figs 1, B, 2, B, and 3, B). The patients were followed up for suture removal at 1 week and re-evaluated at 8 weeks for healing and cosmesis (Figs 1, C, 2, C, and 3, C). Immediate complications included bruising and periorbital swelling in all cases. Cases 1 and 3 resolved within 2 weeks, while case 2 resolved in 1 week. The patient in case 1 was taking 75 mg clopidogrel daily, which was not discontinued prior to surgery. All cases were negative for ectropion development at 6, 12, and 18 months. Evaluation using the Patient and Observer Scar Assessment Scale at 6 months yielded a score of 2 for case 1 and scores of 3 for cases 2 and 3. At 12 months, all scored 1 on the Patient and Observer Scar Assessment Scale.
Discussion
Nasal sidewall defects risk compromised function and cosmesis with postsurgical outcomes. There are several ways to reconstruct the surface of the nose. With adjustments, the Mustardé flap can be used for the closure of nasal primary defects. Specific modifications to the flap are essential to avoid ectropion and nasal contortion. In these patients, the most essential step was the proper placement of the anchoring suture along the zygomatic arch to allow for the utilization of tissue. The skin laxity in these patients also allowed for the modification of the flap to stretch and successfully repair the nasal defect. Skin laxity redistributes tension vectors and closes wounds that are not amenable to primary closure alone.5
The subunits of the nose include the dorsum, tip, columella, paired alae, sidewalls, and soft triangles. The subunit principle proposes the idea that surgically replacing an entire subunit, instead of patching the primary defect, allows scars to be hidden in the contours of the nose and decreases the risk of trapdoor contractions.6 If a trapdoor contraction does occur, subunit replacement forces the contraction to follow the shape of the nasal tip, dorsum, and ala, decreasing its appearance.6 The slight manipulation of the Mustardé flap mimics the crease of the ala, successfully concealing incision lines.
Limitations
The Mustardé technique has notable limitations to discuss. One involves vascular integrity. Patients with histories of smoking, scar tissue from previous surgeries or radiation, and other risks of vascular compromise to the area have the potential for decreased blood supply to the new flaps. Therefore, it is important to consider a patient’s history concerning the potential for vascular complications. Cosmetic preferences also influence the choice of repair method. For example, in men with beards, facial hair could move from its usual preauricular location to the cheek region, limiting the Mustardé flap to patients without facial hair.5 Due to the size of the Mustardé, the risk of ectropion is high; therefore, the specific placement of tracking sutures is essential to redirect tension vectors and avoid the distortion of free margins, most notably on the eyelids and nasal alae. Such challenges may dissuade surgeons who are not familiar with larger facial flaps from choosing the Mustardé flap for nasal repair despite the possibility of excellent outcomes. Physicians should thoroughly discuss all available options that retain the functional operation of the nose while minimizing scarring, ectropion, and surgical dehiscence. Patient comorbidities should also be discussed so that each patient can make an informed decision concerning the approach for nasal reconstruction.
Conclusion
Surgical reconstruction, specifically for large defects on the nose, is challenging. This case series demonstrates the use of the Mustardé flap for achieving positive results in nasal repairs. Historically, the Mustardé flap has been reserved for lower eyelid or cheek primary defect closure after Mohs micrographic surgery. However, this case series demonstrates the successful extension of the Mustardé flap procedure beyond the typical applications to close primary nasal defects. This method illustrates the beneficial aspects of choosing a rotation-advancement flap in terms of redirecting tension to provide functional and aesthetically pleasing outcomes.
Conflicts of interest
None disclosed.
References
1. Badash I, Shauly O, Lui CG, Gould DJ, Patel KM. Nonmelanoma facial skin cancer: a review of diagnostic strategies, surgical treatment, and reconstructive techniques. Clin Med Insights Ear Nose Throat. Published online July 24, 2019. https://doi.org/10.1177/1179550619865278
2. Wong E.Axibal E.Brown M.
Mohs micrographic surgery.
Facial Plast Surg Clin North Am. 2019; 27: 15-34
https://doi.org/10.1016/j.fsc.2018.08.002
3. Ebrahimi A.Ashayeri M. Rasouli HR
Comparison of local flaps and skin grafts to repair cheek skin defects.
J Cutan Aesthet Surg. 2015; 8 : 92-96
https://doi.org/10.4103/0974-2077.158444
4. Austin G.K.Shockley W.W.
Reconstruction of nasal defects: contemporary approaches.
Curr Opin Otolaryngol Head Neck Surg. 2016; 24: 453-460
https://doi.org/10.1097/MOO.0000000000000295
5. Prohaska J, Campos MS, Cook C. Rotation flaps. In: StatPearls [Internet]. StatPearls Publishing; 2021. Accessed December 8, 2021. http://www.ncbi.nlm.nih.gov/pubmed/29493993
6. Search FB
Usefulness of the subunit principle in nasal reconstruction.
An Bras Dermatol. 2017; 92: 159-162
https://doi.org/10.1590/abd1806-4841.20175278
Article Info
Publication History
Published online: March 31, 2022
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
Identification
DOI: https://doi.org/10.1016/j.jdcr.2022.03.014
Copyright
© 2022 by the American Academy of Dermatology, Inc. Published by Elsevier, Inc.
User License
Creative Commons Attribution – NonCommercial – NoDerivs (CC BY-NC-ND 4.0) | How you can reuse
ScienceDirect


Petal Office
Phone:
Fax:
601-336-7826
Address:
Hours of Operation:
Mon-Fri: 8:00am to 4:30pm
Hattiesburg Office
Phone:
Fax:
601-475-9969
Address:
Hours of Operation:
Mon-Fri: 8:00am to 4:30pm
Ellisville Office
Biloxi Office
Phone:
Fax:
228-232-0874
Address:
1009 Tommy Munro Drive, Suite A
Hours of Operation:
Mon-Fri: 8:00am to 4:30pm
Ocean Springs Office
All Rights Reserved | Pine Belt Dermatology